

The government is piloting a screen-and-treat program across seven hospitals and 89 health centers in five districts. The pilot is running until July 2021 and will inform the scale up of cervical cancer care across the country.
The pilot screens women between the ages of 30 and 49 for HPV and aims to reach 70 percent of women living in the targeted districts. All women living with HIV and enrolled in health facilities in the districts will be offered screening, as they are at higher risk of developing cervical cancer.
The screening program focuses on identifying women who need follow-up by one of three methods : HPV DNA testing, Visual Inspection with Acetic acid (VIA), or Pap Smear.
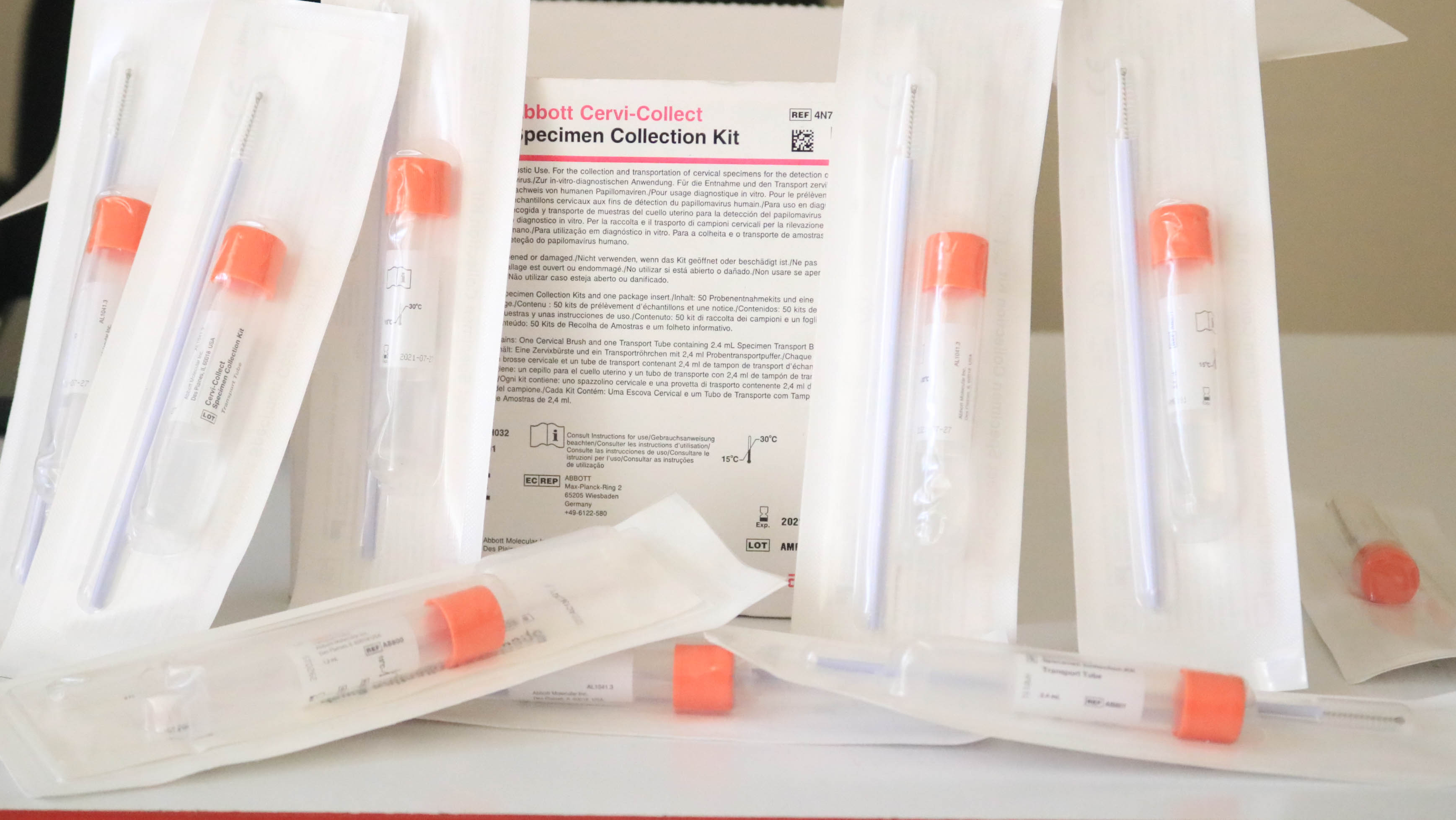
HPV DNA testing is used to check for high-risk HPV infection in women. The sample used for the test is collected from the cervix. The provider may do the test or a self-collection option is available. The sample is then sent to a laboratory where the results will be available in 10 days. The results indicate if the HPV virus is present and if it is a high-risk straintype. If the results are positive for the virus further assessment, such as visual inspection with acetic acid (VIA), are conducted.

When a patient tests positive for HPV, VIA is used to visualise any pre-cancerous lesion on the cervix. It may also be used instead of HPV DNA testing, if that option is not available. The healthcare provider swabs acetic acid on the cervix. Then they look for areas that change colour. Normal cervical tissue remains unaffected by the acetic acid. Damaged tissue — such as that found in pre-cancerous or cancerous lesions — turns white. The provider can then remove the damaged tissue on the spot using minimally invasive techniques such as thermal ablation or other techniques depending on the size of lesions.
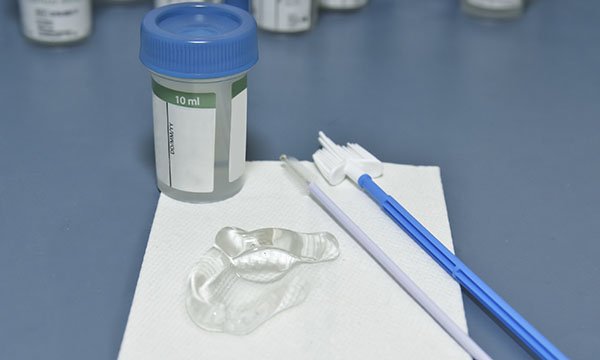
A pap smear, also called a pap test, is another procedure used to test for cervical cancer in women simple test to look for abnormal cells on the cervix. It may be used instead of the HPV DNA and VIA testing combination.
A pap smear involves lightly sweeping the cervix to collect cells for testing. The test is performed in your doctor’s office and takes only a few minutes. After the test, the samples are transferred to a laboratory where they are examined under a microscope to look for characteristics in the cells that indicate cancer or a precancerous condition. Results are usually available in 10 days.
Screening services using HPV DNA testing will soon be offered at all health facilities in five districts. Other districts will continue to provide screening services using VIA or pap smears. For a full list of services available in your area, please visit our Patient Services Page.
Cervical cancer can be prevented by vaccinating girls against HPV and screening and treating women for pre-cancerous lesions.
Rwanda already provides HPV vaccinations to all girls between the ages of 11 and 15.
However, many women born before the immunization program began are not protected and screening rates among this group remains low.
In order to be one of the first countries to eliminate cervical cancer, the government is now piloting
Cervical cancer can be prevented by vaccinating girls against HPV and screening and treating women for pre-cancerous lesions.
Rwanda already provides HPV vaccinations to all girls at the age of 12. The government is now piloting a screen-and-treat program at health centres to catch lesions before they become cancerous.
Cervical cancer is the most common cancer among women in Rwanda. It is caused by a virus called the human papillomavirus or HPV. We can prevent cervical cancer with simple tools such as the HPV vaccine and screening the cervix for disease.
HPV is short for human papillomavirus. HPV causes 99% of cervical cancers.
HPV is spread both sexually and no-sexually, though sexual transmission is the most common route.
Most HPV infections clear up on their own and people don’t even know they have it.
However, certain strains of HPV can cause lesions on the cervix, some of which will turn cancerous if not quickly identified and treated.